Our CEO's Story
Everything started in 2019, when Audry slipped on a set of icy stairs resulting in a sacral fracture. Her first symptoms were lower back pain, terrible headaches and neck/shoulder pain. By the end of 2019, her doctor ordered an MRI after noting an anomaly in a shoulder ultrasound.
That MRI resulted on the finding of a syrinx, which is a cyst inside the spinal cord (Syringomyelia), full of cerebroespinal fluid (CSF) and obstructing the canal. The radiologist also found the fusion of two cervical vertebraes (Klippel-Feil) and led her to see a neurosurgeon who said he didn't have the experience to treat her but assured her symptoms were not related to this finding.
Her symptoms list continued to increase (weakness, numbness, dizziness, palpitations and irregular heart rate) and so the number of doctors she would see, trying to find answers, and that's when she decided to have a consultation with a doctor in the US (in July 2021) who confirmed three diagnoses: Syringomyelia, Klippel-Feil and Tethered Cord. This last anomaly was found on MRI images she had from 2019, which had been seen by several doctors (radiologists, orthopedist, neurosurgeon and family doctor) but none of them were able to see the defect.
By 2023, she had seen around 20 doctors in Canada, had been labeled as a psychiatric patient, had been in the ER at least a dozen of times and had moved to another province, to finally find a Geneticist in Alberta that confirmed the three diseases and, furthermore, ordered a chromosomal microarray wich resulted on a 15q 11.2 deletion, which is also rare and can be responsible for certain neurological conditions.
The full story is told in her first book that will be published soon in Spanish, her native language, and will also be translated and published in English and French next year.

This is how she looks
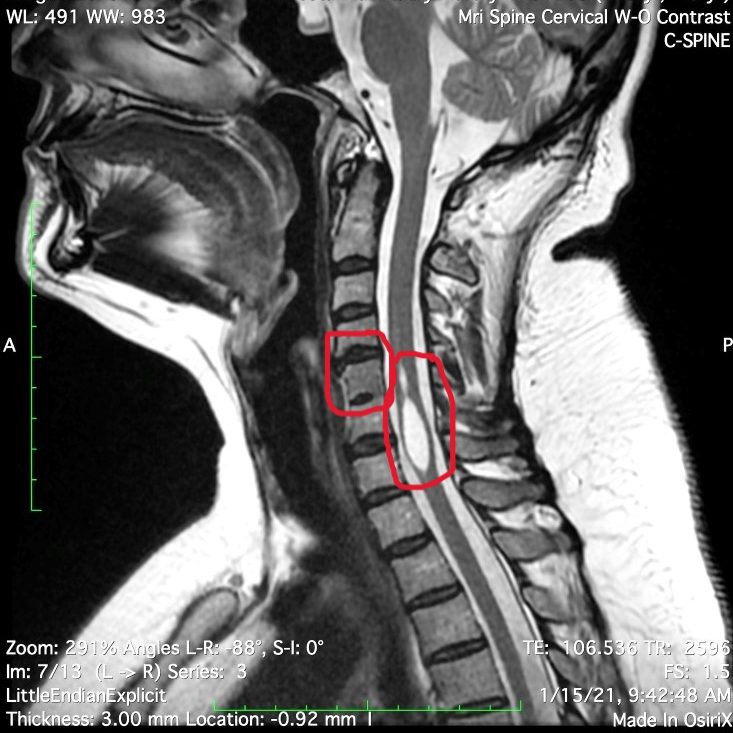
Klippel-Feil shown on the left and
the Syrinx on the right

Tethered Spinal Cord
HER DISEASES
Lets have a closer look to these diseases to have a better understanding of the cause, symptoms and available treatments. Information found on the official website of the National Institute of Health of the United States (www.nih.gov).
SYRINGOMYELIA
Is a neurological disorder in which a fluid-filled cyst (syrinx) forms within the spinal cord. The syrinx can get big enough to damage the spinal cord and compress and injure the nerve fibers that carry information to and from the brain to the body. Some studies have found the prevalence of syringomyelia to be 8.4 cases in 100,000 in the U.S.
In syringomyelia, the watery liquid known as cerebrospinal fluid (CSF)—which surrounds and protects the brain and spinal cord—builds up within the tissue of the spinal cord, expands the central canal, and then forms a syrinx. Generally, a syrinx develops when the normal flow of CSF around the spinal cord or lower brain stem is disturbed. When syrinxes affect the brain stem, the condition is called syringobulbia.
Symptoms of damage to the spinal cord vary among individuals depending on where the syrinx forms, how large it is, and how long it extends. Symptoms develop slowly over time, worsen over many years, and may occur on one or both sides of the body. Symptoms can include:
- Pain (potentially chronic)
- Progressive weakness in arms and legs
- Stiffness in the back, shoulders, neck, arms, or legs
- Headaches
- Loss of sensitivity to pain or hot and cold, especially in the hands
- Numbness or tingling
- Loss of balance
- Loss of bowel and bladder control
- Problems with sexual function
- Curvature of the spine (scoliosis); may be the only symptom in children
Syringomyelia may have several possible causes, but most cases are associated with Chiari malformation—an abnormal condition in which brain tissue extends through the hole at the bottom of the skull (foramen magnum) and into the spinal canal, obstructing the flow of CSF. Syringomyelia may also be caused by spinal cord injuries, spinal cord tumors, and damage caused by inflammation in around the spinal cord. In some cases, the cause is unknown (idiopathic).
There are two major forms of syringomyelia:
- Congenital syringomyelia (also known as communicating syringomyelia) is most often caused by a Chiari malformation and resulting syrinx, usually in the spine's cervical (neck) region. Symptoms typically begin between ages 25 and 40. People with congenital syringomyelia may also have hydrocephalus, a buildup of excess CSF in the brain along with larger than normal connected cavities called ventricles. Straining or coughing can increase the pressure within your head and brain, causing you to develop a headache or even lose consciousness. Some people may have a disorder called arachnoiditis—an inflammation of the arachnoid, one of the three membranes that surrounds the spinal cord.
- Acquired syringomyelia (also known as primary spinal syringomyelia or noncommunicating syringomyelia) can be caused by:
- Spinal cord injury
- Meningitis (an inflammation of brain and spinal cord membranes usually caused by an infection)
- Arachnoiditis
- Tethered cord syndrome (a condition present at birth that causes the spinal cord to abnormally attach to the tissues in the lower spine, limiting its movement)
- Spinal cord tumor
Studies are underway to better understand the role of genetic factors in Chiari I malformation, the most common cause of syringomyelia. Scientists are studying people with a Chiari I malformation who also have a family member with either the abnormality or syringomyelia to identify the location of the gene(s) responsible for the malformation.
In some cases, birth defects may be associated with brain malformations that can cause syringomyelia. Learning how and when these defects occur during fetal development may help scientists develop strategies that can stop the formation of certain birth defects. Folic acid dietary supplements during pregnancy, for example, can reduce the risk of birth defects of the brain and spinal cord.
KLIPPEL-FEIL SYNDROME
Is a rare disorder where two or more vertebrae in the neck are fused together from birth. People living with Klippel-Feil syndrome may have a short neck limited movement, and pain. It is estimated that this syndrome occurs in approximately 1 in 40,000 to 42,000 newborns worldwide.
The most common symptoms of Klippel-Feil syndrome include:
- Short neck and the potential for a low hairline at the back of the head
- Limited flexibility and movement, affecting the face, neck, upper body, and back
- Pain—The fused vertebrae can cause nerve damage and pain in the head, neck, or back
- Hearing loss—Sound signals have a hard time getting to the right part of the ear or brain
People with a certain genetic mutation are at higher risk of developing the disorder. Mutations in the GDF6 (growth differentiation factor 6) or GDF3 (growth differentiation factor 3) genes can cause the disorder.
Doctors usually diagnose Klippel-Feil syndrome at or near birth through observation. Tests may be performed to learn if the disorder is mild or severe.
Doctors currently treat Klippel-Feil syndrome with surgery to correct the neck bones. You may see many types of doctors to treat other symptoms.
People with Klippel-Feil syndrome should avoid activities that can injure the neck. It is possible for people with Klippel-Feil syndrome to live normal lives with proper treatment and care. The outlook depends on the severity of the case and on the number of related conditions a person has.
Unfortunately, Klippel-Feil syndrome is a rare disease and most cases happen without a known cause. This means there is often not much information known about the disorder. Doctors and researchers do not see enough patients with Klippel-Feil Syndrome.
TETHERED CORD SYNDROME
Tethered spinal cord syndrome (TSCS) is a disorder of the nervous system caused by tissue that attaches itself to the spinal cord and limits the movement of the spinal cord. The incidence of the disorder in the general population is still unknown.
The tissue attachments may be present from birth at the base of the spinal cord (known as the conus medullaris), or they may develop near the site of an injury to the spinal cord. They can cause the spinal cord to stretch abnormally.
The course of the disorder is progressive, which means it gets worse as time goes on.
In children, symptoms may include:
- Lesions, hairy patches, dimples, or fatty tumors on the lower back
- Foot and spinal deformities
- Weakness in the legs
- Pain in the lower back
- Scoliosis
- Loss of bowel and bladder control
TSCS in children appears to be caused by incorrect growth of the neural tube while the fetus is developing, and it's related to the disorder called spina bifida.
TSCS may go undiagnosed until adulthood. Symptoms then can include:
- Pain
- Sensory and motor problems
- Loss of bowel and bladder control
These delayed symptoms are related to how much strain is placed on the spinal cord over time. The strain can be made worse during sports or pregnancy, or it may be due to the spinal column get narrower (a process known as stenosis) as a person gets older.
Tethering can also develop after a spinal cord injury. Scar tissue from the injury can block the flow of fluids around the spinal cord. Fluid pressure can then cause cysts to form in the spinal cord, a condition called syringomyelia. This can lead to additional loss of movement, numbness, pain, or other symptoms such as increased heart rate, blood pressure, or problems with breathing.
MRI imaging is often used to evaluate people with symptoms of TSCS. Doctors can use MRI imaging to diagnose where the tethering is located, whether the base of a patient's spinal cord (the conus medullaris) is lower than normal, or if a tumor or a fatty mass (known as a lipoma) is causing the symptoms of TSCS.
In children with TSCS, early surgery is usually recommended to prevent further neurological deterioration. If surgery is not advisable, spinal cord nerve roots may be cut to relieve pain.
In adults, surgery to free (detether) the spinal cord can reduce the size and further development of cysts in the cord. Surgery may also restore some function or alleviate other symptoms. For both children and adults, other forms of treatment can help relieve the symptoms of TSCS.
15q 11.2 MICRODELETION
(Information found on "Unique" official website www.rarechromo.org)
A 15q11.2 deletion is a very rare genetic variation in which there is a tiny piece of chromosome 15 missing. The deletion is found at a place called q11.2. Because the missing piece is very tiny indeed, you will sometimes see it called a microdeletion. What we know about 15q11.2 microdeletions comes from studying people who have a reason for having a genetic test. The reason might be developmental delay, unusual behaviour or a health problem, or perhaps the 15q11.2 microdeletion has been found in someone else in their family. This gives us a biased sample. If we looked for the 15q11.2 microdeletion in the general population, we would have an unbiased sample, but it is very difficult to do. This means that at the moment we can’t be sure about the effect of a 15q11.2 microdeletion. There is still a lot to learn, but this guide contains the best information we have to date. The features of people with a 15q11.2 microdeletion vary widely, even among members of the same family. People can have developmental delay, learning difficulties and behavioural problems. However, many people with the microdeletion have no apparent physical, learning or behaviour difficulties.
Because only very small numbers of people have been identified, we can’t yet be certain what the full range of possible effects of the microdeletion are. Additionally, the features vary, even between members of the same family. They do not affect everyone and in any individual they can be more or less obvious. The most common features are:
- Children may need support with learning. The amount of support needed by each child will vary, although most benefit from supportive services for special needs
- Behaviour and emotional disorders including attention deficit hyperactivity disorder and/or autism in some children
- Speech delay in some children.
Sometimes the 15q11.2 microdeletion can be silent. Some parents of children with a 15q11.2 microdeletion have the same microdeletion but do not have any obvious unusual features or delayed development. The effect on development, health and behaviour of some genetic disorders ranges from being barely perceptible to being obvious and severe.
© Copyright. All rights reserved.
Todos los derechos reservados.
Tous les droits sont réservés.
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details and accept the service to view the translations.
